What is Iron? What does the body use it for?
Iron is the core metal your body uses to move oxygen. It sits at the center of hemoglobin in red blood cells (and myoglobin in muscle), binding oxygen in the lungs and releasing it to your tissues. Beyond oxygen delivery, iron drives cellular energy (it’s built into mitochondrial cytochromes), supports DNA synthesis, and helps your immune system function. Your body tightly regulates iron via the hormone hepcidin, absorbing more when stores are low and less when they’re high, one reason balance matters.
References: NIH ODS Iron fact sheet, Linus Pauling Institute Iron

Health benefits (what adequate iron status supports)
- Steady energy & performance: Iron enables hemoglobin to transport oxygen, sustaining cellular ATP production during everyday activity and exercise.
- Cognitive function: Adequate iron supports attention, learning, and memory; deficiency can impair cognition across the lifespan.
- Healthy pregnancy: Iron needs rise in pregnancy to support maternal blood volume and fetal development; adequacy helps reduce the risk of iron-deficiency anemia.
- Immune readiness: Iron is involved in immune cell proliferation and microbial defense (the body even “locks down” iron during infection).
References: NIH ODSIron:, WHOAnaemia: key facts
How iron interacts with other vitamins,
minerals, and compounds
Iron doesn’t work alone; its absorption and utilization depend on your overall diet:
- Vitamin C (helper): Vitamin C reduces non-heme iron to the more absorbable ferrous form and forms a chelate that’s easier to uptake. Add citrus, peppers, or berries to plant-iron meals.
- “Meat factor” (helper): Amino acids/peptides in meat, fish, and poultry can enhance absorption of non-heme iron eaten in the same meal.
- Calcium (potential inhibitor): Large amounts of calcium (food or supplements) at the same sitting can temporarily reduce iron absorption for that meal; spreading calcium and iron foods/supps apart can help when needed.
- Phytates, polyphenols, soy proteins (inhibitors): Components in bran/legumes (phytate), tea/coffee/cocoa (polyphenols), and some soy proteins can lower non-heme iron absorption. Pairing with vitamin C–rich foods offsets a lot of this.
- Riboflavin (B2) & Vitamin A (enablers): Low riboflavin or vitamin A status can impair iron mobilization, another reason a varied, nutrient-dense diet supports healthy blood indices.
References: LPIIron: enhancers & inhibitors, NIH ODSIron: interactions
Heme vs. plant (non-heme) iron: What’s the difference?
- Heme iron (from animal foods: meat, poultry, seafood) is packaged in hemoglobin/myoglobin and is more readily absorbed, often cited at around 15–35% depending on status. It’s less affected by meal inhibitors.
- Non-heme iron (from plants: legumes, seeds, leafy greens; and most fortified foods) has more variable absorption, roughly 2–20%, strongly influenced by vitamin C, phytate, polyphenols, and overall iron status.
Practically: omnivores typically combine both forms; plant-forward eaters can maximize non-heme iron by adding vitamin C and soaking/sprouting to reduce phytates.
References: LPIIron: heme vs non-heme & absorption ranges, NIH ODSIron: food sources & bioavailability
Low Copper can cause an Iron-Deficiency picture
Copper is a quiet co-star in iron metabolism. Copper-dependent enzymes (ceruloplasmin and hephaestin) oxidize iron to the form that can bind to transferrin and move out of storage sites. With copper deficiency, iron may get “stuck” in tissues and not reach the bone marrow efficiently, leading to anemia that looks like iron deficiency despite adequate iron intake. In such cases, correcting copper, not just adding more iron, is essential.
References: NIH ODSCopper (role in iron transport), LPICopper: interactions with iron
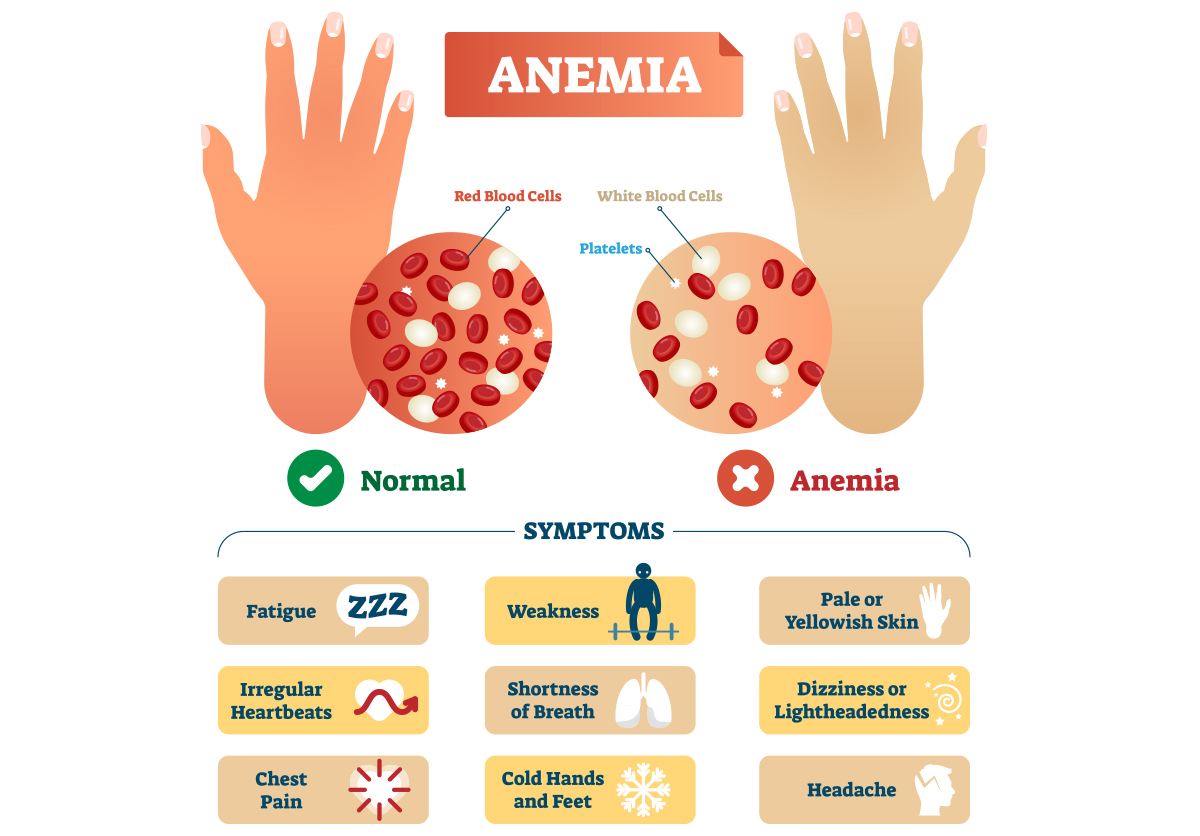
What is anemia?
Anemia is a condition where the hemoglobin or red blood cell count is low, reducing oxygen delivery to tissues. Common signs include fatigue, weakness, pale skin, shortness of breath on exertion, headaches, and poor concentration. There are many types, including iron-deficiency anemia, B12/folate-related megaloblastic anemia, and anemia of chronic inflammation, so testing matters (e.g., CBC, ferritin, transferrin saturation).
References: WHO Anemia overview, NIH ODS Iron: deficiency & assessment
Nutrients that Help Lower the Risk of Anemia
(Beyond Iron itself)
Think “build & deliver” you need the raw materials for red blood cells, plus the cofactors that help iron move and be used correctly:
- Vitamin C: Enhances non-heme iron absorption; aim to pair iron foods with produce like bell peppers, citrus, berries, or broccoli.
Refs: NIH ODSIron interactions, LPIIron - Vitamin A: Supports iron mobilization; deficiency can worsen anemia even with adequate iron.
Refs: LPIVitamin A, WHOVitamin A & anaemia (technical resources) - Folate (B9) & Vitamin B12: Required for DNA synthesis during red blood cell formation; low status causes megaloblastic anemia.
Refs: NIH ODSFolate, NIH ODSB12 - Riboflavin (B2): Low B2 can impair iron utilization and respond to riboflavin repletion.
Refs: LPIRiboflavin & anemia - Copper: Enables iron export and loading onto transferrin (see prior section).
Refs: NIH ODSCopper - Protein & overall calories: Red blood cells are protein-rich; insufficient protein or energy intake can hinder Iron mobilization.
Ref: LPIIron (overview of physiology)
(Medication note: acid-suppressing drugs and certain others can reduce iron absorption or increase losses; individualized guidance from a clinician is wise.)

Whole-food sources highest in iron
Heme (often higher bioavailability):
- Clams (~23 mg per 3 oz, canned), oysters (~8 mg per 3 oz), mussels (~6 mg per 3 oz)
- Grass Fed Beef liver (~5 mg per 3 oz), beef/sirloin (~2–3 mg per 3 oz), sardines (~2 mg per 3 oz), turkey thigh (~2 mg per 3 oz)
Non-heme (pair with whole food vitamin C):
- Lentils, cooked (~6–7 mg per cup), white/navy beans (~5–6 mg per cup), chickpeas (~4–5 mg per cup)
- Pumpkin seeds (~2–3 mg per 1 oz), tahini (~2–3 mg per 2 Tbsp)
- Organic Spinach, cooked (~3 mg per ½ cup), quinoa, cooked (~2–3 mg per cup), blackstrap molasses (~3–4 mg per Tbsp)
Remember: actual absorption depends on your iron status and the meal mix (vitamin C helps; tea/coffee with meals hinders).
References: NIH ODS Iron: food sources
Practical how-to (food-first, then targeted support)
- Build plates that pair iron + C: Chili with beans and tomatoes/peppers; lentil-spinach salad with lemon.
- Mind the timing: If you rely on tea/coffee, enjoy them between iron-rich meals. If you use a calcium supplement, take it at a different mealtime from your iron-rich meal.
- Consider status-guided supplementation: Work with a clinician and labs (ferritin, transferrin saturation, CBC). If you supplement, use gentle, well-absorbed forms from whole foods with cofactors, and avoid unnecessary mega-doses.
- References: NIH ODSIron: deficiency, assessment & supplementation
Safety Snapshot
The Tolerable Upper Intake Level (UL) for supplemental iron in adults is 45 mg/day; excessive iron can cause GI upset and, in overload conditions (e.g., hemochromatosis), organ damage. Keep iron products away from children. Acute overdose is dangerous.
Reference: NIH ODSIron: safety/ULs
Bottom line
Iron is the oxygen-carrier mineral that keeps energy, cognition, and resilience online. A whole-food pattern rich in seafood or lean meats (heme) or legumes, seeds, leafy greens (non-heme) + vitamin C covers most needs, and when anemia risk is present, check the supporting cast: copper, vitamins A/C/B2/B9/B12, adequate protein, and overall diet quality.
The Supporting Cast Supplements from NAHS: Keep Iron Levels Up
Purely Liver: Vitamin A, essential amino acid proteins, B9, B12, Heme Iron, Copper
Purely C: Raw, wholefood vitamin C with Bioflavonoids, Quercetin, Copper
Purely B: Vitamin B complex with Antioxidants and trace Minerals
Purely Zinc Plus: Good source of whole food Iron, Magnesium, Zinc, Copper, and vitamin C
Explore our trending products:
-
Herbal-zzZs – Melatonin-Free Sleep Support
$31.99 — or subscribe to save 15% Add to cart -
Black Seed-Plus Capsules
$29.99 — or subscribe to save 15% Select options This product has multiple variants. The options may be chosen on the product page -
Purely-C Whole Food Vitamin C Complex
$37.99 — or subscribe to save 15% Select options This product has multiple variants. The options may be chosen on the product page -
PurelyMin Magnesium Complex
$39.99 — or subscribe to save 15% Add to cart